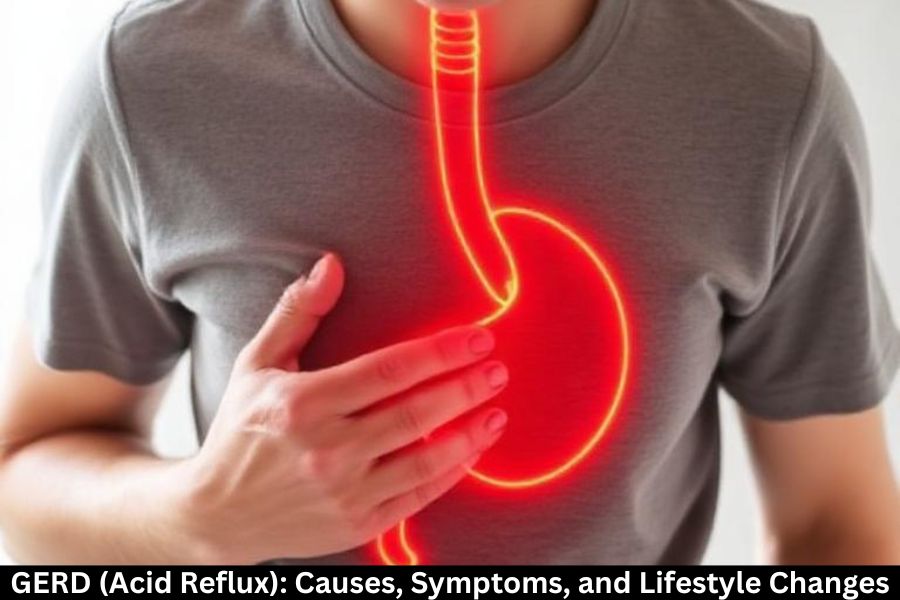
Living with frequent heartburn or constant indigestion can be incredibly uncomfortable. If you’ve ever felt that burning sensation rise from your stomach to your chest after eating, you’re not alone. This could be a sign of GERD, also known as Gastroesophageal Reflux Disease. It’s one of the most common digestive disorders globally, affecting millions each year.
In this article, we’ll break down what GERD is, why it happens, what symptoms to look out for, and how you can control it using lifestyle changes, home remedies, and medical treatments.
What Is GERD?
GERD occurs when stomach acid flows back into the esophagus repeatedly, causing irritation and discomfort. This happens when the lower esophageal sphincter (LES)—a small muscle between the esophagus and stomach—doesn’t close properly.
Think of the LES as a one-way door. When it becomes weak or damaged, acid sneaks through and causes that burning sensation.
How Common Is GERD?
GERD affects people of all ages—from children to older adults. It’s especially common in people who are overweight, pregnant, or lead a sedentary lifestyle. With dietary habits shifting globally, GERD cases are increasing each year.
What Causes GERD?
Weakening of the Lower Esophageal Sphincter (LES)
This is the main trigger. When the LES is weak or relaxes at the wrong time, acid reflux occurs.
Dietary Factors
Certain foods and beverages relax the LES or boost acid production, including:
- Citrus fruits
- Spicy dishes
- Chocolate
- Coffee
- Fatty foods
- Alcohol
Medical Conditions
Some health issues contribute to GERD, such as:
- Hiatal hernia
- Obesity
- Pregnancy
- Diabetes
- Connective tissue disorders
Lifestyle Influences
Daily habits can play a huge role. These include:
- Smoking
- Eating large meals
- Eating close to bedtime
- Lack of physical activity
- Stress
Common Symptoms of GERD
Frequent Heartburn
A burning feeling in the chest, especially after meals or at night.
Acid Regurgitation
A sour or bitter taste when acid or food returns to the mouth.
Chest Pain and Discomfort
Often mistaken for heart-related issues, GERD chest pain worsens when lying down.
Difficulty Swallowing (Dysphagia)
Narrowing of the esophagus due to inflammation can make swallowing hard.
Chronic Cough and Throat Issues
Acid can irritate the throat, causing:
- Persistent cough
- Hoarseness
- Throat soreness
- Postnasal drip sensation
GERD Complications
If not treated, GERD can cause serious health issues.
Esophagitis
Chronic acid exposure inflames and damages the esophagus lining.
Barrett’s Esophagus
A precancerous condition where the esophagus lining changes.
Respiratory Issues
Acid entering the airways can lead to:
- Asthma flare-ups
- Bronchitis
- Shortness of breath
Diagnosis of GERD
Doctors use several tests to confirm GERD:
Physical Examination
Symptoms alone often give a strong indication.
Endoscopy
A camera is inserted to view the esophagus for inflammation or damage.
pH Monitoring
Measures the acidity levels in the esophagus.
Esophageal Manometry
Determines if the esophagus muscles are working properly.
Lifestyle Changes to Manage GERD
Small adjustments can make a massive difference.
Dietary Adjustments
Avoid foods that trigger reflux, and include:
- Lean proteins
- Whole grains
- Vegetables
- Non-citrus fruits
Healthy Eating Habits
- Eat smaller meals
- Avoid eating 2–3 hours before bed
- Chew food thoroughly
- Drink water throughout the day
Weight Management
Losing even a few pounds can reduce pressure on the stomach.
Sleeping Position and Bed Elevation
Raise the head of your bed 6–8 inches to prevent nighttime reflux.
Stress Management
Activities like yoga, deep breathing, and meditation reduce flare-ups.
Home Remedies for GERD Relief
Herbal Options
- Ginger tea
- Chamomile
- Licorice root (DGL)
Natural Supplements
- Aloe vera juice (in moderation)
- Slippery elm
- Probiotics
Safe Everyday Practices
- Wear loose clothing
- Stay upright after meals
- Avoid heavy lifting right after eating
Medical Treatments
Over-the-Counter Medications
- Antacids
- H2 blockers
- Proton pump inhibitors (PPIs)
Prescription Drugs
Used for severe or chronic GERD.
Surgical Options
If medications fail, doctors may recommend procedures like:
- Fundoplication
- LINX device implantation
Preventing GERD Flare-Ups
Foods to Avoid
- Tomatoes
- Peppermint
- Carbonated drinks
- Garlic and onions
Habits to Break
- Lying down immediately after eating
- Overeating
- Smoking
Living With GERD
Managing GERD is all about balance. With the right lifestyle changes and treatments, most people can control symptoms effectively and avoid serious complications. It’s about understanding your triggers, making conscious choices, and being consistent.
Conclusion
GERD may be uncomfortable, but it’s far from unbeatable. By understanding its causes and symptoms, you can take charge of your digestive health. Simple lifestyle changes alone can dramatically improve your condition, while medical treatments offer strong support if needed. Listen to your body, avoid known triggers, and make adjustments that support long-term wellness.
FAQs
Can GERD go away on its own?
Mild cases may improve with lifestyle changes, but chronic GERD often needs treatment.
Is GERD the same as heartburn?
No—heartburn is a symptom; GERD is a chronic digestive disorder.
How is GERD different from acid reflux?
Acid reflux is occasional; GERD is frequent or severe reflux.
Can drinking water help GERD?
Yes, water can dilute stomach acid and soothe symptoms temporarily.
Is GERD dangerous?
Untreated GERD can lead to complications like esophagitis or Barrett’s esophagus.