Endometriosis is a chronic and often painful condition that affects millions of women worldwide. Yet, despite how common it is, many people go years without a proper diagnosis. The symptoms can be confusing, the pain often dismissed, and the emotional toll can be overwhelming. This article breaks down everything you need to know—symptoms, causes, diagnosis methods, and treatment options—to help you understand and manage this condition more confidently.
What Is Endometriosis?
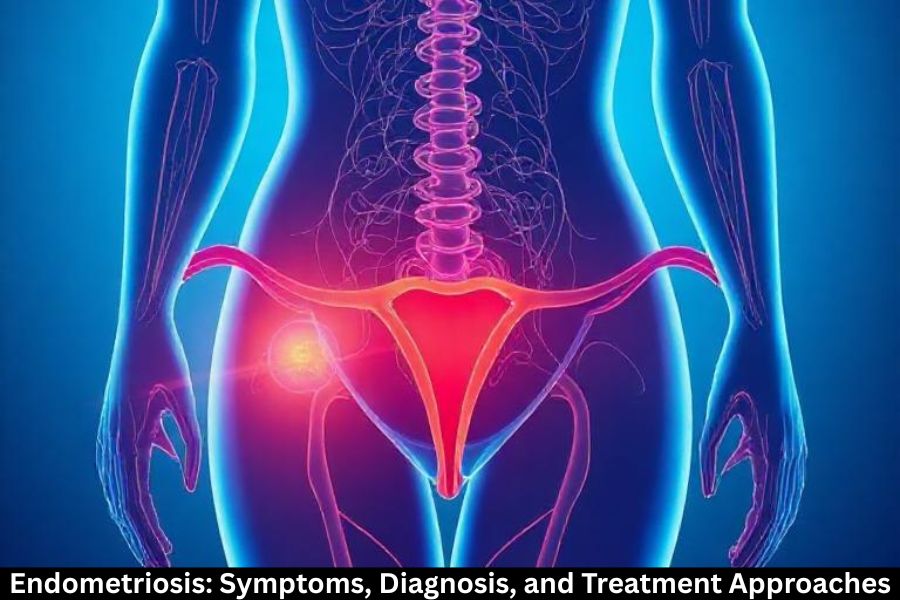
Endometriosis happens when tissue similar to the lining of the uterus (called the endometrium) grows outside the uterus. These growths can appear on the ovaries, fallopian tubes, bladder, intestines, and other organs in the pelvic area. Because this tissue behaves like normal uterine lining, it thickens, breaks down, and bleeds during the menstrual cycle. But since it has nowhere to go, it leads to inflammation, pain, and scar tissue.
How Common Is It?
Endometriosis affects roughly 1 in 10 women of reproductive age. Many go undiagnosed for years because symptoms are often mistaken for normal menstrual cramps or other conditions like IBS.
Who Is at Risk?
Anyone who menstruates can develop endometriosis, but risk is higher in women:
- With a family history of the condition
- Who have early menstruation
- With heavy or long periods
- Who have never given birth
Causes and Risk Factors
Possible Causes of Endometriosis
The exact cause remains unknown, but several theories exist:
- Retrograde menstruation: Menstrual blood flows backward into the pelvic cavity.
- Genetic tendencies: It often runs in families.
- Immune system issues: The body may fail to eliminate displaced endometrial cells.
Genetic Factors
If your mother or sister has endometriosis, your risk is significantly higher, suggesting a hereditary component.
Hormonal Influences
Estrogen plays a major role in the growth of endometriosis lesions, which is why hormonal therapies can help manage symptoms.
Lifestyle and Environmental Factors
High stress, poor diet, and exposure to toxins may contribute to inflammation, making symptoms worse.
Symptoms of Endometriosis
Pelvic Pain
The most common symptom. Pain may feel sharp, stabbing, or persistent.
Painful Periods (Dysmenorrhea)
Many women with endometriosis experience severe cramping that interferes with daily activities.
Pain During Intercourse
Deep penetration can irritate affected areas, causing intense discomfort.
Digestive Symptoms
Bloating, diarrhea, constipation, and nausea—especially during periods—are common.
Infertility
Endometriosis can affect fertility by causing scarring and altering reproductive anatomy.
How Endometriosis Affects the Body
Inflammation and Scar Tissue
The trapped blood and tissue cause inflammation, which leads to scar tissue over time.
Formation of Endometriomas
These are cysts filled with old blood, often found on the ovaries.
Adhesions and Their Impact
Scar tissue can cause organs to stick together, leading to severe pain and complications.
Diagnosis of Endometriosis
Medical History and Physical Exam
Doctors start by reviewing symptoms and performing a pelvic exam.
Imaging Tests
Ultrasound
Useful for identifying ovarian cysts but not always effective in detecting small lesions.
MRI
Provides a clearer view of pelvic structures and helps plan surgery when needed.
Laparoscopy as the Gold Standard
A minimally invasive surgery that allows doctors to see and remove endometriosis lesions.
Why Endometriosis Is Often Misdiagnosed
Symptoms overlap with IBS, pelvic inflammatory disease, and menstrual disorders, leading many women to go undiagnosed for years.
Treatment Approaches
Medications
Pain Relievers
NSAIDs like ibuprofen can reduce inflammation and pain.
Hormonal Therapies
Birth control pills, progesterone therapies, and GnRH agonists help slow endometrial growth.
Surgical Options
Laparoscopic Excision
The most effective surgery for removing lesions while preserving fertility.
Hysterectomy (Rare Cases)
Used only when other treatments fail and symptoms are severe.
Assisted Reproductive Technologies (ART)
For women struggling with infertility, IVF may be an effective option.
Alternative and Complementary Treatments
Acupuncture, yoga, and dietary changes can help manage chronic pain.
Lifestyle Changes That Help Manage Symptoms
Diet and Nutrition
Reducing red meat, caffeine, and processed foods may decrease inflammation. Anti-inflammatory diets often help reduce flare-ups.
Exercise and Stress Relief
Low-impact exercise like yoga or swimming releases endorphins and eases pain.
Heat Therapy
Heating pads can relax muscles and reduce cramps.
Sleep and Daily Habits
Maintaining a consistent sleep schedule supports hormone balance and overall well-being.
Living With Endometriosis
Emotional and Mental Health
Chronic pain can affect mood, relationships, and self-esteem. Therapy and support groups can make a big difference.
Support Groups and Resources
Connecting with others reduces feelings of isolation and helps you find practical coping strategies.
Long-Term Outlook
While there’s no cure yet, many women manage symptoms effectively through a combination of treatments and lifestyle changes.
Conclusion
Endometriosis is a complex condition that affects millions of women, yet it is still widely misunderstood. Recognizing the symptoms, seeking timely diagnosis, and exploring the right treatment options can transform your quality of life. With proper medical care, lifestyle adjustments, and emotional support, it is absolutely possible to manage endometriosis and live a healthier, more comfortable life.
FAQs
Can endometriosis be cured?
There is no cure yet, but symptoms can be managed with medications, surgery, and lifestyle changes.
Does endometriosis always cause infertility?
No. Many women with endometriosis can conceive naturally or with medical support.
Can diet help with symptoms?
Yes. Anti-inflammatory foods like leafy greens, berries, and omega-3-rich fish may reduce flare-ups.
How long does diagnosis usually take?
On average, it takes 7–10 years for many women to receive an accurate diagnosis.
Is surgery always necessary?
Not always. Surgery is recommended when symptoms are severe or when fertility is affected.